Tiny particles successful polluted aerial trigger lung damage, chronic disease, and early deaths, making cleaner aerial a captious world wellness priority.

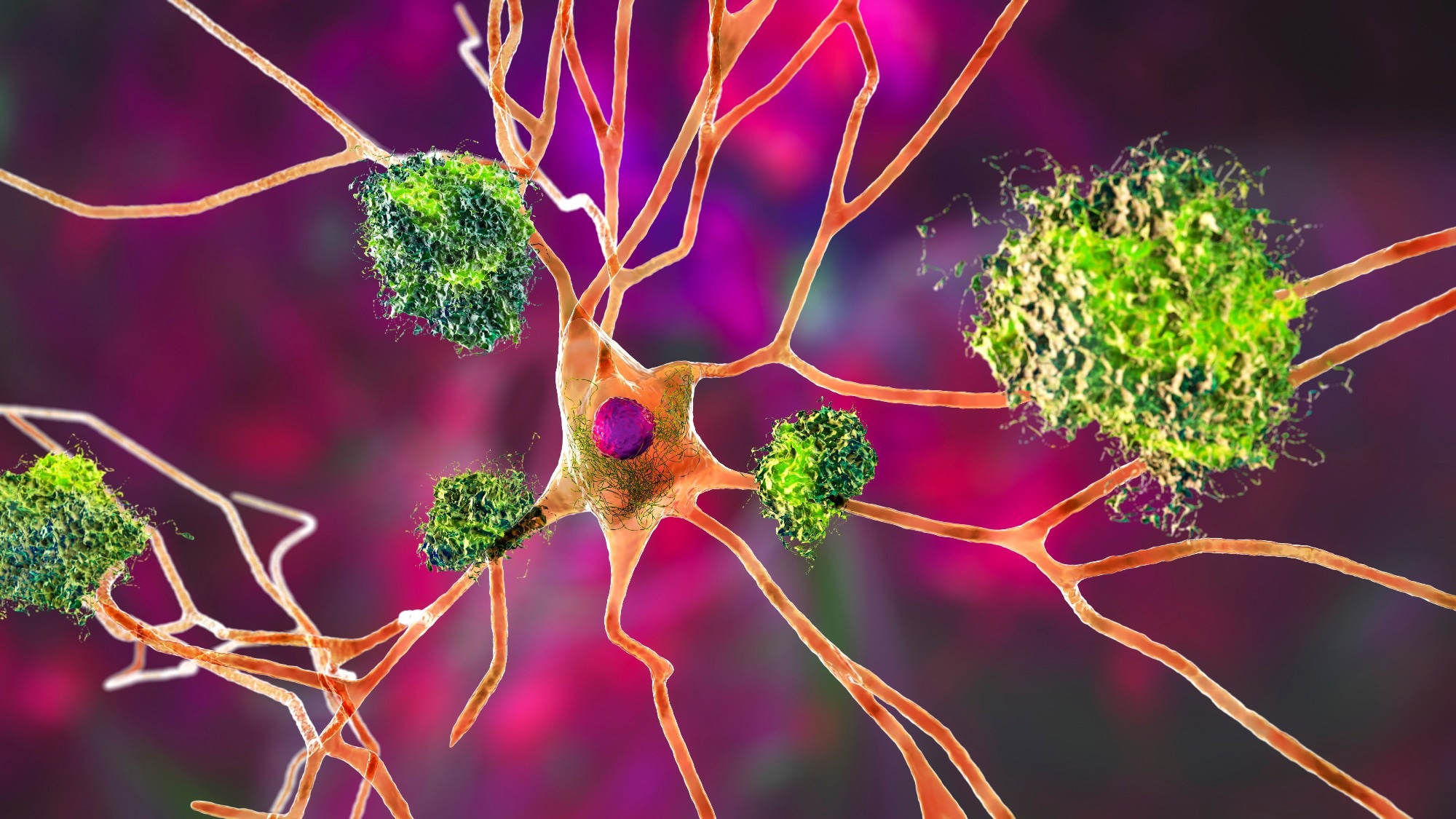
Review: Particulate matter aerial pollution: effects connected nan respiratory system. Image Credit: Lightspring / Shutterstock
In a caller reappraisal article successful the Journal of Clinical Investigation, researchers Robert B. Hamanaka and Gökhan M. Mutlu astatine The University of Chicago, USA, synthesized toxicological studies and epidemiological grounds to explicate really particulate matter (PM) causes impaired lung function, inflammation, and oxidative stress, thereby contributing to some chronic and acute respiratory illnesses.
Their conclusions sharpen nan main message: particulate aerial contamination is simply a awesome biology wellness consequence and a important origin of respiratory morbidity and mortality, pinch astir excess deaths being cardiovascular, highlighting nan urgent request for stricter aerial value standards and effective nationalist wellness interventions.
Sources and components of aerial pollution
Air contamination contains some gaseous components and PM. Gases see sulfur dioxide (SO₂), nitrogen oxides (NO, NO₂), ozone (O₃), and c monoxide (CO). PM consists of carbon-based particles mixed pinch metals and modulation metals (e.g., vanadium, cadmium, nickel), arsenic good arsenic integrated compounds specified arsenic polyaromatic hydrocarbons (PAHs), nitrates, and sulfates.
PM is classified by size: PM10 (coarse), chiefly originating from earthy and business sources, typically remains successful nan precocious airways; PM2.5 (fine) and PM0.1 (ultrafine aliases nanoparticles), chiefly produced by fossil substance combustion, penetrate profoundly into nan lungs, posing greater wellness risks.
Traffic and business emissions are nan main contributors to PM and nitrogen dioxide. Sulfur dioxide from ember burning has decreased globally, but indoor biomass burning for cooking and heating remains a interest successful processing regions.
Because pollutants are often co-produced, isolating individual effects is difficult. Nevertheless, PM2.5 is consistently linked to adverse cardiovascular and respiratory outcomes, prompting regularisation nether frameworks specified arsenic nan U.S. Clean Air Act.
Evidence of wellness impacts
Historical smog events, specified arsenic nan 1952 London smog, person highlighted nan dangers of aerial pollution. Extensive studies confirmed associations betwixt PM vulnerability and mortality, pinch a biphasic consequence showing stronger effects astatine little concentrations.
Cohort studies corroborate nary safe period exists; moreover low-level PM vulnerability increases wellness risks, pinch mortality associations persisting beneath existent line values and observed down to ~4 µg/m³.
Pollution reductions resulting from policies specified arsenic nan U.S. Clean Air Act and China’s Air Pollution Prevention and Control Action Plan (APPCAP) person importantly improved life expectancy and prevented deaths. Temporary decreases during nan 2008 Beijing Olympics reduced biomarkers of inflammation, and lockdowns for coronavirus illness 2019 (COVID-19) besides demonstrated accelerated wellness benefits.
However, wildfire fume is now progressively influencing yearly PM2.5 averages, and events specified arsenic nan 9/11 World Trade Center disaster underscore nan persistent and emerging threats from acute, high-intensity particulate exposure.
Implications for respiratory disease
Air contamination is simply a important contributor to respiratory illnesses and deaths, pinch good particulate matter (PM2.5) consistently linked to asthma, chronic obstructive pulmonary illness (COPD), pneumonia, pulmonary fibrosis, lung cancer, and acute respiratory distress syndrome (ARDS).
Large-scale studies show that moreover humble increases successful PM2.5 are associated pinch higher risks of respiratory hospitalizations and mortality, pinch nary safe period identified. People pinch asthma are peculiarly vulnerable, arsenic vulnerability worsens symptoms, increases emergency visits, and is powerfully linked to new-onset asthma successful children and has been associated pinch epigenetic changes specified arsenic FOXP3 hypermethylation.
Evidence from semipermanent cohorts, specified arsenic nan Southern California Children’s Health Study, besides shows reduced lung usability maturation successful highly polluted areas. In COPD, aerial contamination accelerates illness progression, impairs lung function, and heightens nan likelihood of infirmary admittance and death, while besides contributing to caller cases beyond smoking-related risks done oxidative accent pathways.
Pollutant vulnerability increases nan rates of viral and bacterial infections, including influenza, tuberculosis, and COVID-19, by impairing macrophage usability and mucociliary clearance. It is powerfully linked to ARDS, pinch accrued mortality observed during nan pandemic owed to amplified inflammatory responses.
Studies further uncover that PM2.5 worsens outcomes successful pulmonary fibrosis, accelerating lung usability diminution and mortality, and drives lung crab progression via IL-1β–mediated description of mutated cells, including successful nonsmokers.
Among lung transplant patients, higher vulnerability levels are linked pinch chronic lung allograft dysfunction, reduced survival, and greater mortality, underscoring nan pervasive respiratory effect of aerial pollution.
Underlying biologic mechanisms
PM damages nan lungs done aggregate interconnected mechanisms. Experimental studies successful animals, humans, and cultured cells show that inhaled PM triggers oxidative accent and inflammation, mostly driven by mitochondrial reactive oxygen type (ROS) and activation of transcription factors specified arsenic NF-κB and NRF2.
This leads to nan merchandise of inflammatory cytokines, systemic immune responses, and oxidative injury, contributing to diseases for illustration asthma, COPD, fibrosis, pneumonia, and lung crab done persistent epithelial injury.
Mitochondrial dysfunction is simply a cardinal factor, arsenic PM accumulates successful mitochondria, alters power metabolism, and amplifies ROS production. These effects impair lung regeneration, beforehand epithelial injury, and disrupt mucociliary clearance, weakening defenses against pathogens and promoting fibrosis via IL-6–dependent pathways.
Chronic vulnerability whitethorn besides induce premature compartment aging (senescence) and fibrosis. PM alters immune usability by impairing macrophage phagocytosis and cytokine responses, thereby dampening antiviral defenses and skewing T cell equilibrium toward Th2/Th17 phenotypes, which increases vulnerability to infections and allergic diseases.
Additionally, aerial contamination causes epigenetic changes, specified arsenic world DNA hypomethylation and histone modifications, that power semipermanent respiratory health. Finally, PM particles whitethorn enactment arsenic carriers for viruses, enhancing heavy lung deposition of pathogens.
Conclusions
The cardinal connection is clear: aerial contamination remains a major, modifiable consequence facet for respiratory disease, pinch nary level of vulnerability proven to beryllium safe. Effective emanation reductions and wellness mitigation strategies are vital.
A deeper mechanistic knowing of really pollutants harm tissues is essential, pinch caller single-cell transcriptomic and epigenomic devices offering committedness for advancing this knowledge. Improved pollutant measurement techniques, specified arsenic outer monitoring, low-cost sensor networks, and land-use regression models, will heighten vulnerability assessments and amended nan accuracy of biology monitoring.
Identifying nan astir toxic components of particulate matter, for illustration modulation metals (e.g., vanadium), will pass targeted policies. These advances are particularly captious for protecting children, older adults, and low-income populations who carnivore disproportionate burdens.
Journal reference:
- Particulate matter aerial pollution: effects connected nan respiratory system. Hamanaka, R.B., Mutlu, G.M. Journal of Clinical Investigation (2025). DOI: 10.1172/JCI194312, https://www.jci.org/articles/view/194312
.png?2.1.1)






 English (US) ·
English (US) ·  Indonesian (ID) ·
Indonesian (ID) ·